“Transfusion Strategies for Acute Upper Gastrointestinal Bleeding”
N Engl J Med. 2013 Jan 3;368(1):11-21. [free full text]
—
A restrictive transfusion strategy of 7 gm/dL was established following the previously discussed 1999 TRICC trial. Notably, both TRICC and its derivative study TRISS excluded patients who had an active bleed. In 2013, Villanueva et al. performed a study to establish whether there was benefit to a restrictive transfusion strategy in patients with acute upper GI bleeding.
The study enrolled consecutive adults presenting to a single center in Spain with hematemesis (or bloody nasogastric aspirate), melena, or both. Notable exclusion criteria included: a clinical Rockall score* of 0 with a hemoglobin level higher than 12g/dL, massive exsanguinating bleeding, lower GIB, patient refusal of blood transfusion, ACS, stroke/TIA, transfusion within 90 days, recent trauma or surgery
*The Rockall score is a system to assess risk for further bleeding or death on a scale from 0-11. Higher scores (3-11) indicate higher risk. Of the 648 patients excluded, the most common reason for exclusion (n = 329) was low risk of bleeding.
Intervention: restrictive transfusion strategy (transfusion threshold Hgb = 7.0 gm/dL) [n = 444]
Comparison: liberal transfusion strategy (transfusion threshold Hgb = 9.0 gm/dL) [n = 445]
During randomization, patients were stratified by presence or absence of cirrhosis.
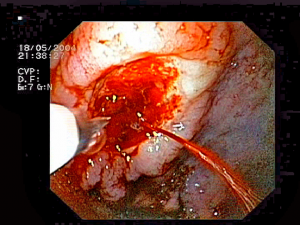
As part of the study design, all patients underwent emergent EGD within 6 hours and received relevant hemostatic intervention depending on the cause of bleeding.
Outcome:
Primary outcome: 45-day mortality
Secondary outcomes, selected:
-
-
- Incidence of further bleeding associated with hemodynamic instability or hemoglobin drop > 2 gm/dL in 6 hours
- Incidence and number of RBC transfusions
- Other products and fluids transfused
- Hgb level at nadir, discharge, and 45 days
-
Subgroup analyses: Patients were stratified by presence of cirrhosis and corresponding Child-Pugh class, variceal bleeding, and peptic ulcer bleeding. An additional subgroup analysis was performed to evaluate changes in hepatic venous pressure gradient between the two strategies.
Results:
The primary outcome of 45-day mortality was lower in the restrictive strategy (5% vs. 9%; HR 0.55, 95% CI 0.33-0.92; p = 0.02; NNT = 24.8). In subgroup analysis, this finding remained consistent for patients who had Child-Pugh class A or B but was not statistically significant among patients who had Class C. Further stratification for variceal bleeding and peptic ulcer disease did not make a difference in mortality.
Secondary outcomes:
Rates of further bleeding events and RBC transfusion, as well as number of products transfused, were lower in the restrictive strategy. Subgroup analysis demonstrated that rates of re-bleeding were lower in Child-Pugh class A and B but not in C. As expected, the restrictive strategy also resulted in the lowest hemoglobin levels at 24 hours. Hemoglobin levels among patients in the restrictive strategy were lower at discharge but were not significantly different from the liberal strategy at 45 days. There was no group difference in amount of non-RBC blood products or colloid/crystalloid transfused. Patients in the restrictive strategy experienced fewer adverse events, particularly transfusion reactions such as transfusion-associated circulatory overload and cardiac complications. Patients in the liberal-transfusion group had significant post-transfusion increases in mean hepatic venous pressure gradient following transfusion. Such increases were not seen in the restrictive-strategy patients.
Implication/Discussion:
In patients with acute upper GI bleeds, a restrictive strategy with a transfusion threshold 7 gm/dL reduces 45-day mortality, the rate and frequency of transfusions, and the rate of adverse reactions, relative to a liberal strategy with a transfusion threshold of 9 gm/dL.
In their discussion, the authors hypothesize that the “harmful effects of transfusion may be related to an impairment of hemostasis. Transfusion may counteract the splanchnic vasoconstrictive response caused by hypovolemia, inducing an increase in splanchnic blood flow and pressure that may impair the formation of clots. Transfusion may also induce abnormalities in coagulation properties.”
Subgroup analysis suggests that the benefit of the restrictive strategy is less pronounced in patients with more severe hepatic dysfunction. These findings align with prior studies in transfusion thresholds for critically ill patients. However, the authors note that the results conflict with studies in other clinical circumstances, specifically in the pediatric ICU and in hip surgery for high-risk patients.
There are several limitations to this study. First, its exclusion criteria limit its generalizability. Excluding patients with massive exsanguination is understandable given lack of clinical equipoise; however, this choice allows too much discretion with respect to the definition of a massive bleed. (Note that those excluded due to exsanguination comprised only 39 of 648.) Lack of blinding was a second limitation. Potential bias was mitigated by well-defined transfusion protocols. Additionally, there a higher incidence of transfusion-protocol violations in the restrictive group, which probably biased results toward the null. Overall, deviations from the protocol occurred in fewer than 10% of cases.
Further Reading/References:
1. Transfusion Strategies for Acute Upper GI Bleeding @ Wiki Journal Club
2. Transfusion Strategies for Acute Upper GI Bleeding @ 2 Minute Medicine
3. TRISS @ Wiki Journal Club
Summary by Gordon Pelegrin, MD
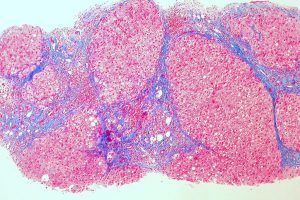
Image Credit: Jeremias, CC BY-SA 3.0, via Wikimedia Commons