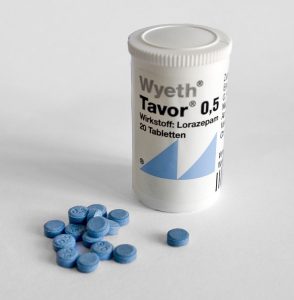
“Symptom-Triggered vs Fixed-Schedule Doses of Benzodiazepine for Alcohol Withdrawal”
Arch Intern Med. 2002 May 27;162(10):1117-21. [free full text]
—
Treatment of alcohol withdrawal with benzodiazepines has been the standard of care for decades. However, in the 1990s, benzodiazepine therapy for alcohol withdrawal was generally given via fixed doses. In 1994, a double-blind RCT by Saitz et al. demonstrated that symptom-triggered therapy based on responses to the CIWA-Ar scale reduced treatment duration and the amount of benzodiazepine used relative to a fixed-schedule regimen. This trial had little immediate impact in the treatment of alcohol withdrawal. The authors of the 2002 double-blind RCT sought to confirm the findings from 1994 in a larger population that did not exclude patients with a history of seizures or severe alcohol withdrawal.
The trial enrolled consecutive patients admitted to the inpatient alcohol treatment units at two European universities (excluding those with “major cognitive, psychiatric, or medical comorbidity”) and randomized them to treatment with either scheduled placebo (30mg q6hrs x4, followed by 15mg q6hrs x8) with additional PRN oxazepam 15mg for CIWA score 8-15 and 30mg for CIWA score > 15 or to treatment with scheduled oxazepam (30mg q6hrs x4, followed by 15mg q6hrs x8) with additional PRN oxazepam 15mg for CIWA score 8-15 and 30mg for CIWA score > 15.
The primary outcomes were cumulative oxazepam dose at 72 hours and duration of treatment with oxazepam. Subgroup analysis included the exclusion of symptomatic patients who did not require any oxazepam. Secondary outcomes included incidence of seizures, hallucinations, and delirium tremens at 72 hours.
Results:
117 patients completed the trial. 56 had been randomized to the symptom-triggered group, and 61 had been randomized to the fixed-schedule group. The groups were similar in all baseline characteristics except that the fixed-schedule group had on average a 5-hour longer interval since last drink prior to admission. While only 39% of the symptom-triggered group actually received oxazepam, 100% of the fixed-schedule group did (p < 0.001). Patients in the symptom-triggered group received a mean cumulative dose of 37.5mg versus 231.4mg in the fixed-schedule group (p < 0.001). The mean duration of oxazepam treatment was 20.0 hours in the symptom-triggered group versus 62.7 hours in the fixed-schedule group. The group difference in total oxazepam dose persisted even when patients who did not receive any oxazepam were excluded. Among patients who did receive oxazepam, patients in the symptom-triggered group received 95.4 ± 107.7mg versus 231.4 ± 29.4mg in the fixed-dose group (p < 0.001). Only one patient in the symptom-triggered group sustained a seizure. There were no seizures, hallucinations, or episodes of delirium tremens in any of the other 116 patients. The two treatment groups had similar quality-of-life and symptom scores aside from slightly higher physical functioning in the symptom-triggered group (p < 0.01). See Table 2.
Implication/Discussion:
Symptom-triggered administration of benzodiazepines in alcohol withdrawal led to a six-fold reduction in cumulative benzodiazepine use and a much shorter duration of pharmacotherapy than fixed-schedule administration. This more restrictive and responsive strategy did not increase the risk of major adverse outcomes such as seizure or DTs and also did not result in increased patient discomfort.
Overall, this study confirmed the findings of the landmark study by Saitz et al. from eight years prior. Additionally, this trial was larger and did not exclude patients with a prior history of withdrawal seizures or severe withdrawal. The fact that both studies took place in inpatient specialty psychiatry units limits their generalizability to our inpatient general medicine populations.
Why the initial 1994 study did not gain clinical traction remains unclear. Both studies have been well-cited over the ensuing decades, and the paradigm has shifted firmly toward symptom-triggered benzodiazepine regimens using the CIWA scale. While a 2010 Cochrane review cites only the 1994 study, Wiki Journal Club and 2 Minute Medicine have entries on this 2002 study but not on the equally impressive 1994 study.
Further Reading/References:
1. “Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial.” JAMA. 1994.
2. Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar)
3. Wiki Journal Club
4. 2 Minute Medicine
5. “Benzodiazepines for alcohol withdrawal.” Cochrane Database Syst Rev. 2010
Summary by Duncan F. Moore, MD
Image Credit: VisualBeo, CC BY-SA 3.0, via Wikimedia Commons