“Prednisolone or Pentoxifylline for Alcohol Hepatitis”
aka the Steroids or Pentoxifylline for Alcoholic Hepatitis (STOPAH) trial
N Engl J Med. 2015 Apr 23;372(17):1619-28. [free full text]
—
Severe alcoholic hepatitis is associated with short-term mortality as high as 30%. Treatment of alcoholic hepatitis with corticosteroids has been extensively studied and debated. Prior to this 2010 study, an analysis of the five largest studies of glucocorticoid treatment in alcoholic hepatitis concluded that there was a significant mortality benefit at 28 days among patients with severe disease. Similarly, the nonselective phosphodiesterase inhibitor pentoxifylline has been evaluated in alcoholic hepatitis. One of four RCTs showed a significant benefit, but two meta-analyses have not concluded that there is any benefit. The authors of the 2010 STOPAH trial sought to evaluate both therapies compared to placebos in a 2-by-2 factorial design.
The trial enrolled adults with a clinical diagnosis of alcoholic hepatitis, average alcohol consumption > 80 gm/day in men or 60 gm/day in women, total bilirubin > 4.7mg/dL, and a Maddrey discriminant function ≥ 32 [https://www.mdcalc.com/maddreys-discriminant-function-alcoholic-hepatitis]. Patients were randomized to one of the following four groups for 28 days of treatment.
-
-
- prednisolone-matched placebo daily + pentoxifylline-matched placebo TID
- prednisolone 40mg daily + pentoxifylline-matched placebo TID
- prednisolone-matched placebo daily + pentoxifylline 400mg TID
- prednisolone 40mg placebo daily + pentoxifylline 400mg TID
-
The primary outcome was 28-day mortality. The major secondary outcome was mortality or liver transplant at 90 days and at 1 year.
Regarding randomization of the 1103 patients, 276 were randomized to placebo-placebo, 277 to prednisolone-placebo, 276 to pentoxifylline-placebo, and 274 to prednisolone-pentoxifylline. The trial was stopped early due to “limitations on funding.” However, all enrolled patients completed at least 28 days of follow-up. 33 patients were unable to complete 90-day and 1-year follow-up due to termination of the trial.
At 28 days, 45 of 269 (17%) of placebo-placebo patients, 38 of 266 (14%) of prednisolone-placebo patients, 50 of 258 (19%) of pentoxifylline-placebo patients, and 35 of 260 (13%) of prednisolone-pentoxifylline patients had died. The odds ratio for 28-day mortality among patients treated with prednisolone was 0.72 (95% CI 0.52-1.01, p = 0.06), and the odds ratio for patients treated with pentoxifylline was 1.07 (95% CI 0.77-1.49, p = 0.69).
Similarly, neither treatment was found to influence 90-day or 1-year mortality or liver transplantation. (See Table 2.) Infection occurred in 13% of patients who received prednisolone versus 7% of patients who did not receive prednisolone.
Implication/Discussion:
In patients with severe alcoholic hepatitis, neither prednisolone nor pentoxifylline reduced morality risk at 28 days. Additionally, neither drug reduced the combined secondary endpoint of mortality or liver transplantation at 90 days or 1 year.
This was a well-designed, randomized, double-blind, double-placebo-controlled trial. A notable limitation was this trial’s reliance on the clinical diagnosis of alcohol hepatitis, rather than tissue diagnosis. This may have reduced the power of the trial with respect to detecting a treatment effect. Contemporary authors also noted that harm may have come to study patients due to a lack of tapering of prednisolone at the end of the 28 days of treatment.
A 2015 meta-analysis that included the STOPAH trial concluded that prednisolone treatment reduced 28-day mortality.
Despite the negative results of this specific trial, corticosteroid treatment has remained a mainstay of the treatment of severe alcoholic hepatitis.
The generally accepted practice, as summarized by UpToDate, is treatment with prednisolone 40mg PO daily for 28 days in patients with discriminant function ≥ 32. (Prednisolone is preferred over prednisone because prednisone requires conversion in the liver to its active form prednisolone, and such conversion can be impaired in liver dysfunction.) Therapy should be terminated early after 7 days if patients fail to show improvement (either by parameters such as bilirubin or discriminant function or by improvement in the Lille score).
Further Reading/References:
1. STOPAH @ Wiki Journal Club
2. STOPAH @ 2 Minute Medicine
3. UpToDate, “Management and prognosis of alcoholic hepatitis”
4. American College of Gastroenterology, “ACG Clinical Guideline: Alcoholic Liver Disease” (2018)
5. European Association for Study of the Liver (EASL), “EASL Clinical Practice Guidelines: Management of Alcoholic Liver Disease” (2012)
Summary by Duncan F. Moore, MD
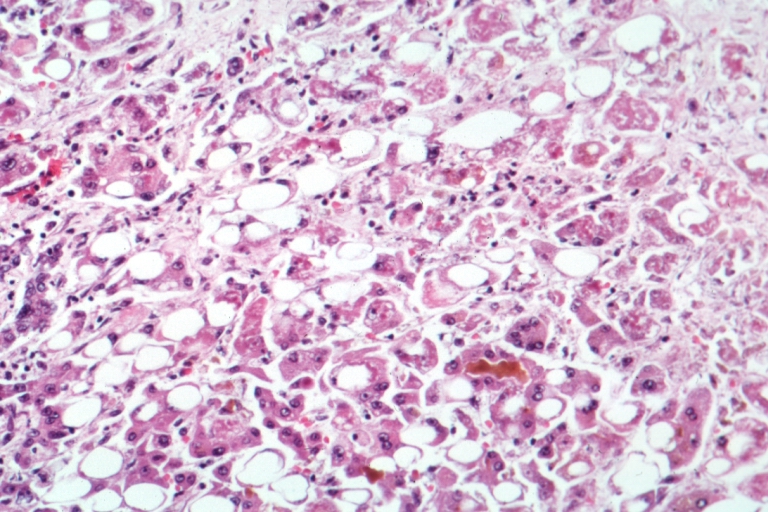
Image Credit: University of Alabama at Birmingham Department of Pathology, CC BY-SA 2.5, via Wikimedia Commons