“A Multicenter, Randomized, Controlled Clinical Trial of Transfusion Requirements in Critical Care”
N Engl J Med. 1999 Feb 11; 340(6): 409-417. [free full text]
—
Although intuitively a hemoglobin closer to normal physiologic concentration seems like it would be beneficial, the vast majority of the time in inpatient settings we use a hemoglobin concentration of 7g/dL as our threshold for transfusion in anemia. Historically, higher hemoglobin cutoffs were used with aims to keep Hgb > 10g/dL. In 1999, the landmark TRICC trial demonstrated no mortality benefit in the liberal transfusion strategy and harm in certain subgroup analyses.
Population:
Inclusion: critically ill patients expected to be in ICU > 24h, Hgb ≤ 9g/dL within 72hr of ICU admission, and clinically euvolemic after fluid resuscitation
Exclusion criteria: age < 16, inability to receive blood products, active bleed, chronic anemia, pregnancy, brain death, consideration of withdrawal of care, and admission after routine cardiac procedure.
Patients were randomized to either a liberal transfusion strategy (transfuse to Hgb goal 10-12g/dL, n = 420) or a restrictive strategy (transfuse to Hgb goal 7-9g/dL, n = 418). The primary outcome was 30-day all-cause mortality. Secondary outcomes included 60-day all-cause mortality, mortality during hospital stay (ICU plus step-down), multiple-organ dysfunction score, and change in organ dysfunction from baseline. Subgroup analyses included APACHE II score ≤ 20 (i.e. less-ill patients), patients younger than 55, cardiac disease, severe infection/septic shock, and trauma.
Results:
The primary outcome of 30-day mortality was similar between the two groups (18.7% vs. 23.3%, p = 0.11). The secondary outcome of mortality rate during hospitalization was lower in the restrictive strategy (22.2% vs. 28.1%, p = 0.05). (Of note, the mean length of stay was about 35 days for both groups.) 60-day all-cause mortality trended towards lower in the restrictive strategy although did not reach statistical significance (22.7% vs. 26.5 %, p = 0.23). Between the two groups, there was no significant difference in multiple-organ dysfunction score or change in organ dysfunction from baseline.
Subgroup analyses in patients with APACHE II score ≤ 20 and patients younger than 55 demonstrated lower 30-day mortality and lower multiple-organ dysfunction score among patients treated with the restrictive strategy. In the subgroups of primary disease process (i.e. cardiac disease, severe infection/septic shock, and trauma) there was no significant differences among treatment arms.
Complications in the ICU were monitored, and there was a significant increase in cardiac events (primarily pulmonary edema) in the liberal strategy group when compared to the restrictive strategy group.
Discussion/Implication:
The TRICC trial demonstrated that, among ICU patients with anemia, there was no difference in 30-day mortality between a restrictive and liberal transfusion strategy. Secondary outcomes were notable for a decrease in inpatient mortality with the restrictive strategy. Furthermore, subgroup analyses showed benefit in various metrics for a restrictive transfusion strategy when adjusting for younger and less ill patients. This evidence laid the groundwork for our current standard of transfusing to hemoglobin 7g/dL. A restrictive strategy has also been supported by more recent studies. In 2014 the Transfusion Thresholds in Septic Shock (TRISS) study showed no change in 90-day mortality with a restrictive strategy. Additionally, in 2013 the Transfusion Strategy for Acute Upper Gastrointestinal Bleeding study showed reduced 40-day mortality in the restrictive strategy. However, the study’s exclusion of patients who had massive exsanguination or low rebleeding risk reduced generalizability. Currently, the Surviving Sepsis Campaign endorses transfusing RBCs only when Hgb < 7g/dL unless there are extenuating circumstances such as MI, severe hypoxemia, or active hemorrhage.
Further reading:
1. TRICC @ Wiki Journal Club
2. TRICC @ 2 Minute Medicine
3. TRISS @ Wiki Journal Club, full text, Georgetown Critical Care Top 40 pages 14-15
4. “Transfusion strategies for acute upper gastrointestinal bleeding” (NEJM 2013) @ 52 in 52 (2018-2019) Week 41, @ Wiki Journal Club, full text
5. “Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2016”
Summary by Gordon Pelegrin, MD
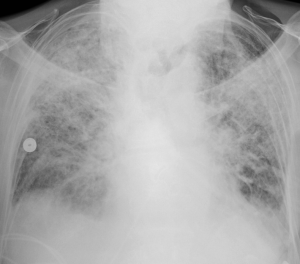
Image Credit: U.S. Air Force Master Sgt. Tracy L. DeMarco, public domain, via WikiMedia Commons