“A Novel User-Friendly Score (HAS-BLED) To Assess 1-Year Risk of Major Bleeding in Patients with Atrial Fibrillation”
Chest. 2010 Nov;138(5):1093-100. [free full text]
—
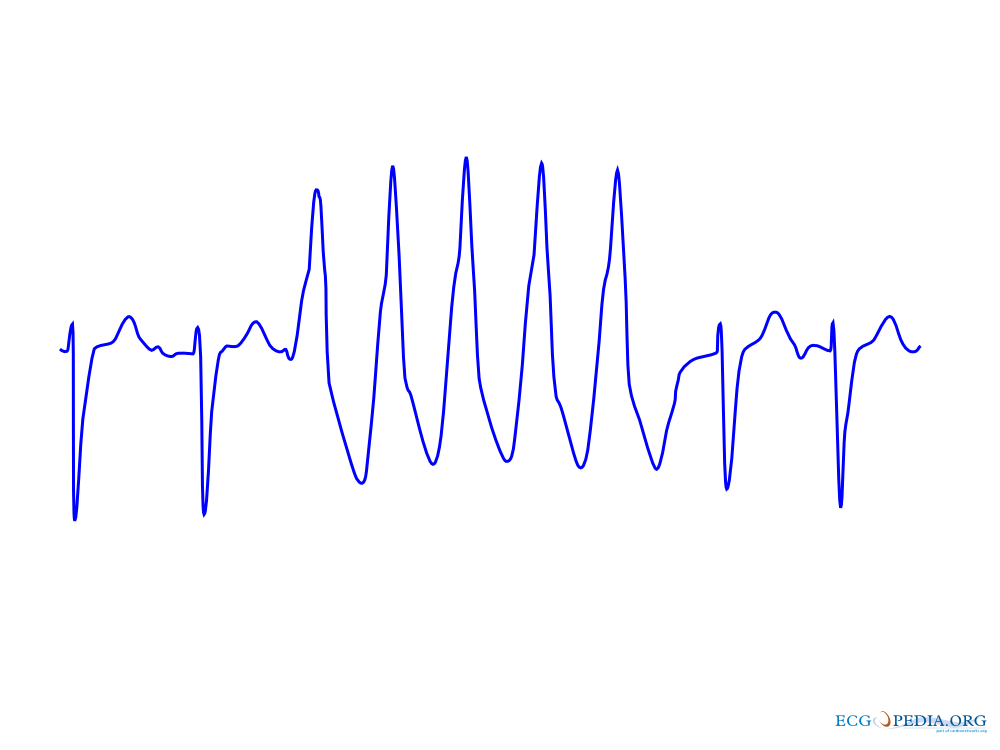
Atrial fibrillation (AF) is a well-known risk factor for ischemic stroke. Stroke risk is further increased by individual comorbidities such as CHF, HTN, and DM and can be stratified with scores such as CHADS2 and CHA2DS2VASC. The recommendation for patients with intermediate stroke risk is treatment with oral anticoagulation (OAC). However, stroke risk is often closely related to bleeding risk, and the benefits of anticoagulation for stroke need to be weighed against the added risk of bleeding. At the time of this study, there were no validated and user-friendly bleeding risk-stratification schemes. This study aimed to develop a practical risk score to estimate the 1-year risk of major bleeding (as defined in the study) in a contemporary, real-world cohort of patients with AF.
Population: adults with EKG or Holter-proven diagnosis of AF
Exclusion criteria: mitral valve stenosis, valvular surgery
(Patients were identified from the prospectively developed database of the multi-center Euro Heart Survey on AF. Among 5,272 patients with AF, 3,456 were free of mitral valve stenosis or valve surgery and completed their 1-year follow-up assessment.)
No experiment was performed in this retrospective cohort study.
In a derivation cohort, the authors retrospectively performed univariate analyses to identify a range of clinical features associated with major bleeding (p < 0.10). Based on systematic reviews, they added additional risk factors for major bleeding. Ultimately, the result was a list of comprehensive risk factors that make up the acronym HAS-BLED:
H – Hypertension (> 160 mmHg systolic)
A – Abnormal renal (HD, transplant, Cr > 2.26 mg/dL) and liver function (cirrhosis, bilirubin >2x normal w/ AST/ALT/ALP > 3x normal) – 1 pt each for abnormal renal or liver function
S – Stroke
B – Bleeding (prior major bleed or predisposition to bleed)
L – Labile INRs (time in therapeutic range < 60%)
E – Elderly (age > 65)
D – Drugs (i.e. ASA, clopidogrel, NSAIDs) or alcohol use (> 8 units per week) concomitantly – 1 pt each for use of either
Each risk factor represents one point each. The HAS-BLED score was then compared to the HEMORR2HAGES scheme, a previously developed tool for estimating bleeding risk.
Outcomes:
- incidence of major bleeding within 1 year
- bleeds per 100 patient-years, stratified by HAS-BLED score
- c-statistic for the HAS-BLED score in predicting the risk of bleeding
Definitions:
- major bleeding: bleeding causing hospitalization, Hgb drop >2 g/L, or bleeding requiring blood transfusion (excluded hemorrhagic stroke)
- hemorrhagic stroke: focal neurologic deficit of sudden onset that is diagnosed by a neurologist, lasting > 24h, and caused by bleeding
Results:
3,456 AF patients (without mitral valve stenosis or valve surgery) who completed their 1-year follow-up were analyzed retrospectively. 64.8% (2242) of these patients were on OAC (with 12.8% (286) of this subset on concurrent antiplatelet therapy), 24% (828) were on antiplatelet therapy alone, and 10.2% (352) received no antithrombotic therapy. 1.5% (53) of patients experienced a major bleed during the first year. 17% (9) of these patients sustained intracerebral hemorrhage.
HAS-BLED Score Bleeds per 100-patient years
0 1.13
1 1.02
2 1.88
3 3.74
4 8.70
5 12.50
6* 0.0 *(n = 2 patients at risk, neither bled)
Patients were given a HAS-BLED score and a HEMORR2HAGES score. C-statistics were then used to determine the predictive accuracy of each model overall as well as within patient subgroups (OAC alone, OAC + antiplatelet, antiplatelet alone, and no antithrombotic therapy).
C statistics for HAS-BLED:
For overall cohort, 0.72 (95% CI 0.65-0.79); for OAC alone, 0.69 (95% CI 0.59-0.80); for OAC + antiplatelet, 0.78 (95% CI 0.65-0.91); for antiplatelet alone, 0.91 (95% CI 0.83-1.00); and for those on no antithrombotic therapy, 0.85 (95% CI 0.00-1.00).
C statistics for HEMORR2HAGES:
For overall cohort, 0.66 (95% CI 0.57-0.74); for OAC alone, 0.64 (95% CI 0.53-0.75); for OAC + antiplatelet, 0.83 (95% CI 0.74-0.91); for antiplatelet alone, 0.83 (95% CI 0.68-0.98); and for those on no antithrombotic therapy, 0.81 (95% CI 0.00-1.00).
Implication/Discussion:
This study helped to establish a practical and user-friendly assessment of bleeding risk in AF. HAS-BLED is superior to its predecessor HEMORR2HAGES because the acronym is easier to remember, the assessment is quicker and simpler to perform, and all risk factors are readily available from the clinical history or routine testing. Both stratification tools had (grossly) similar c-statistics for the overall cohort – 0.72 for HAS-BLED versus 0.66 for HEMORR2HAGES. However, HAS-BLED was particularly useful when looking at antiplatelet therapy alone or no antithrombotic therapy at all (0.91 and 0.85, respectively).
This study is useful because it provides evidence-based, easily calculable, and actionable risk stratification in the assessment of bleeding risk in AF. In prior studies, such as ACTIVE-A (ASA + clopidogrel versus ASA alone for patients with AF deemed unsuitable for OAC), almost half of all patients (n= ~3500) were given a classification of “unsuitable for OAC,” which was based solely on physicians’ clinical judgement without a predefined objective scoring. Now, physicians have an objective way to assess bleed risk rather than “gut feeling” or wanting to avoid iatrogenic insult.
The RE-LY trial used the HAS-BLED score to decide which patients with AF should get the standard dabigatran dose (150mg BID) rather than a lower dose (110mg BID) for anticoagulation. This risk-stratified dosing resulted in a significant reduction in major bleeding compared with warfarin but maintained a similar reduction in stroke risk.
Furthermore, the HAS-BLED score could allow the physician to be more confident when deciding which patients may be appropriate for referral for a left atrial appendage occlusion device (e.g. Watchman).
Limitations:
The study had a limited number of major bleeds and a short follow-up period, and thus it is possible that other important risk factors for bleeding were not identified. Also, there were large numbers of patients lost to 1-year follow-up. These patients likely had more comorbidities and may have transferred to nursing homes or even died. Their loss to follow-up and thus exclusion from this retrospective study may have led to an underestimate of true bleeding rates. Furthermore, generalizability is limited by the modest number of very elderly patients (i.e. 75-84 and ≥85), who likely represent the greatest bleeding risk. Finally, this study did not specify what proportion of its patients were on warfarin for their OAC, but given that dabigatran, rivaroxaban, and apixaban were not yet approved for use in Europe (2008, 2008, and 2011, respectively) for the majority of the study, we can assume most patients were on warfarin. Thus the generalizability of HAS-BLED risk stratification to the DOACs is limited.
Bottom Line:
HAS-BLED provides an easy, practical tool to assess the individual bleeding risk of patients with AF. Oral anticoagulation should be considered for scores of 3 or less. If HAS-BLED scores are ≥4, it is reasonable to think about alternatives to oral anticoagulation.
Further Reading/References:
1. 2 Minute Medicine
2. ACTIVE-A trial
3. RE-LY trial
4. RE-LY @ Wiki Journal Club
5. HAS-BLED Calculator
6. HEMORR2HAGES Calculator
7. Watchman (for Healthcare Professionals)
Summary by Patrick Miller, MD